After the murder of George Floyd on May 25, 2020, and the national reckoning that ensued, CCMH immediately began to explore ways students could share recent experiences of discrimination when they seek services at college counseling centers. This initiative was deemed critical by the collective collegiate mental health community given the CCMH measures at the time did not adequately capture experiences of discrimination from the student’s perspective, and there was cautious optimism this awareness raising effort would help clinicians more effectively comprehend the contextual environments of students and enhance the support services they provide. Moreover, research emphasizing that discrimination is connected to increased mental health distress, social isolation, and suicidality (Oh et al., 2018; Paradies et al., 2015) further highlighted the need for this endeavor.
After one year of piloting questions to address this goal, CCMH officially implemented the following Yes/No questions as part of the National Standardized Data Set (SDS) – Client Information form on July 1, 2021: “In the past 6 months, have you experienced discrimination or unfairtreatment due to any of the following parts of your identity? (Disability, Gender, Nationality/Country of Origin, Race/Ethnicity/Culture, Religion, Sexual Orientation).”
It should be clearly understood at the outset that the experience of discrimination is not a mental health diagnosis. Discrimination is a societal problem that needs to be addressed, and concurrently, it is essential to assess how these experiences are associated with mental health concerns. The 2023 Annual Report specifically investigated if discrimination or unfair treatment based on any of the six identities described above is associated with mental health symptoms and how college counseling centers support students who have experienced discrimination.
The following questions were explored:
- Are student’s experiences of discrimination associated with higher baseline levels of general distress, social isolation, and suicidal ideation?
- Compared to other clinical variables that are routinely gathered at the beginning of treatment (e.g., history of suicide attempts, prior treatment), what is the strength of the relationship between discrimination and presenting symptoms of general distress, social isolation, and suicidal ideation?
- Do students with experiences of discrimination demonstrate improvement in general distress, social isolation, and suicidal ideation during college counseling services that is comparable to clients who do not report discrimination?
Data related to discrimination were collected from the CCMH Standardized Data Set (SDS) – Client Information form, while general distress, social isolation, and suicidal ideation was assessed using the Counseling Center Assessment of Psychological Symptoms (CCAPS) measure. Both of these self-report tools are typically implemented when students initiate services at college counseling centers nationally. Additionally, the CCAPS is commonly administered throughout treatment to monitor progress.
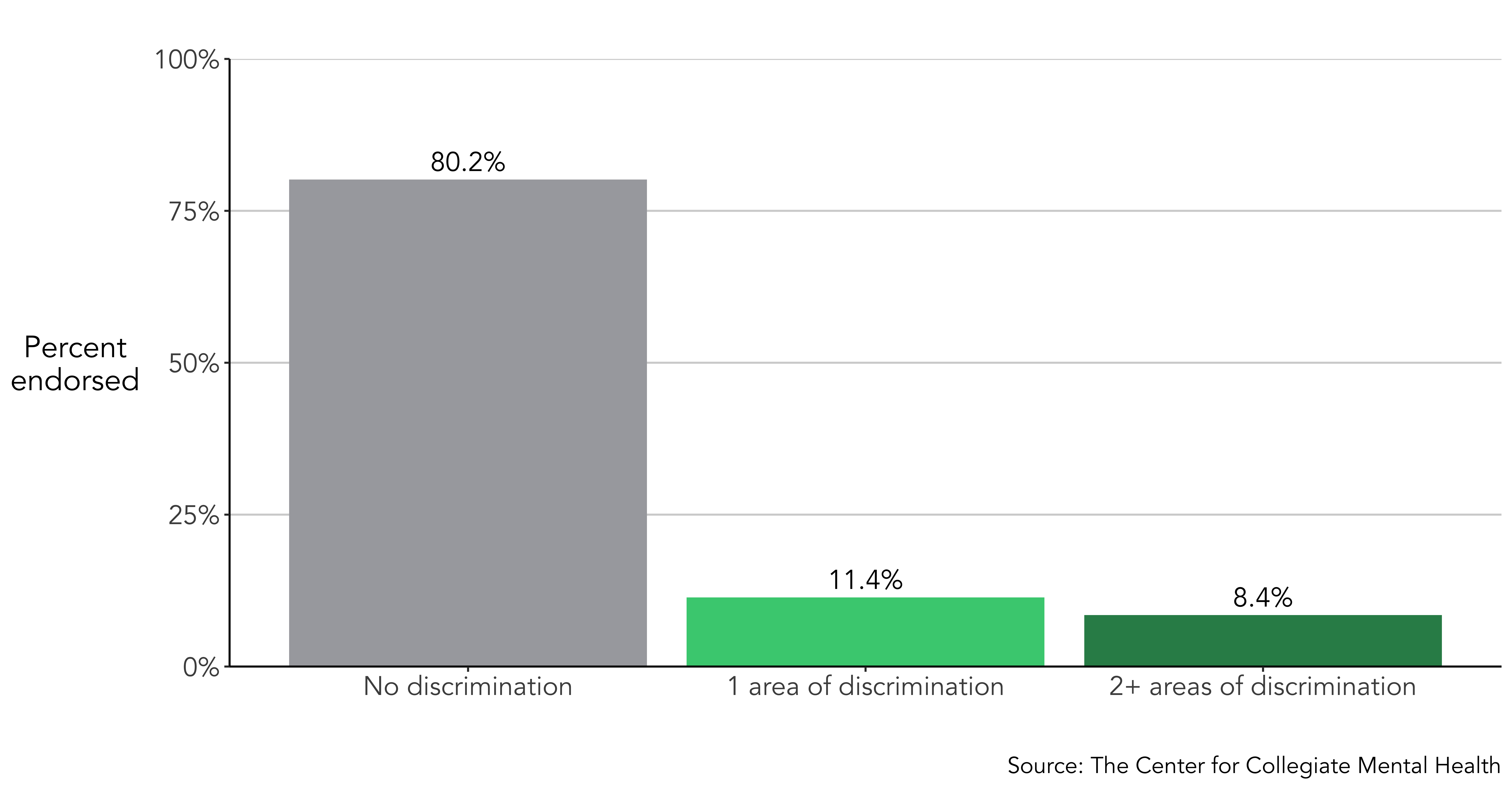
Data for the current Annual Report include 78,432 students who were treated at 85 different college counseling centers nationally from 2021 to 2023. Overall, 19.8% of all students disclosed experiencing discrimination in the past six months based on 1 or more identities when they entered counseling services, while 8.4% reported discrimination in multiple (2+) identity areas.
DISCRIMINATION AND GENERAL DISTRESS, SOCIAL ISOLATION, AND SUICIDALITY
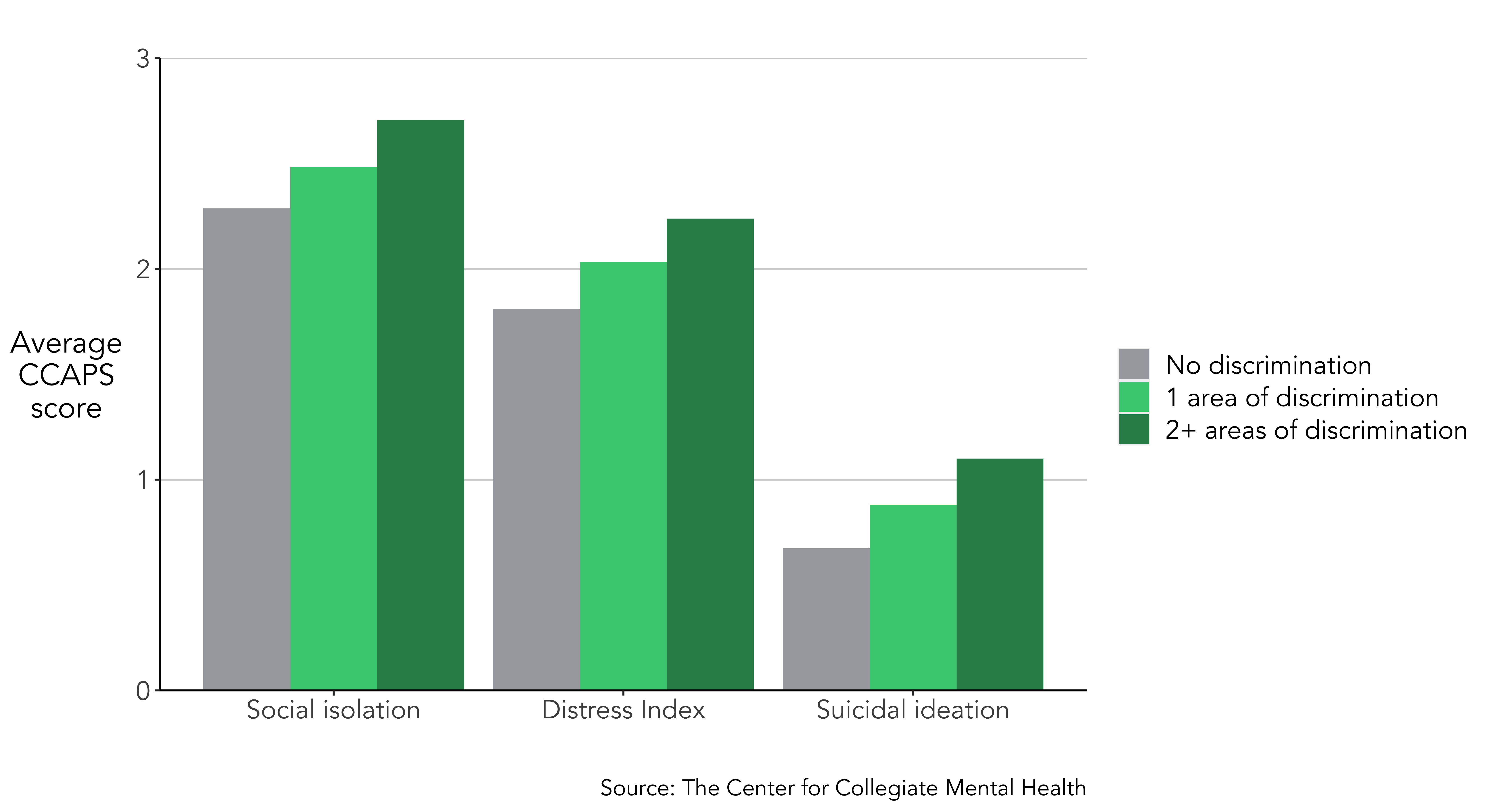
CCMH explored if students who share experiences of discrimination demonstrate higher levels of general distress, social isolation, and suicidal ideation compared to clients who do not report discrimination. Students who acknowledged discrimination based on 1 or multiple (2+) identities within the past six months reported substantially higher general distress, social isolation, and suicidal thoughts at the outset of counseling services. Furthermore, if students experienced multiple areas of discrimination, they displayed greater levels of distress, isolation, and suicidal ideation than students with either no discrimination or only 1 area.
DISCRIMINATION COMPARED TO TRADITIONAL CLINICAL HISTORY VARIABLES
Clinicians traditionally have been trained to gather specific information regarding a client’s clinical history when they enter treatment. Among other things, this typically includes an assessment of prior mental health treatment, risk-related variables (i.e., suicidal behavior), and trauma. Information pertaining to a client’s clinical history provides valuable data that typically corresponds with their level of presenting distress and informs the subsequent treatment plan.
In the current Annual Report, CCMH examined how experiences of discrimination compare to these traditional clinical history variables in terms of their association with general distress, social isolation, and suicidal ideation. These comparisons should be interpreted with the understanding that discrimination is not a mental health problem. Rather, they are presented to illustrate how recent discrimination may impact a client’s presenting symptoms in comparison to clinical variables that providers have been trained to routinely collect. Specifically, we examined the following clinical history variables:
- Prior counseling or therapy
- Prior substance use treatment
- Prior psychotropic medication
- Prior psychiatric hospitalization
- History of trauma
- History of non-suicidal self-injury
- History of suicide attempt(s)
When students complete the SDS Client Information form at the outset of treatment, there are a wide range of responses they can provide, including endorsing any combination of the clinical history variables and types of discrimination. Thus, these items are not mutually exclusive, where a client could endorse both clinical history and discrimination experiences, either of these variables, or none of them.
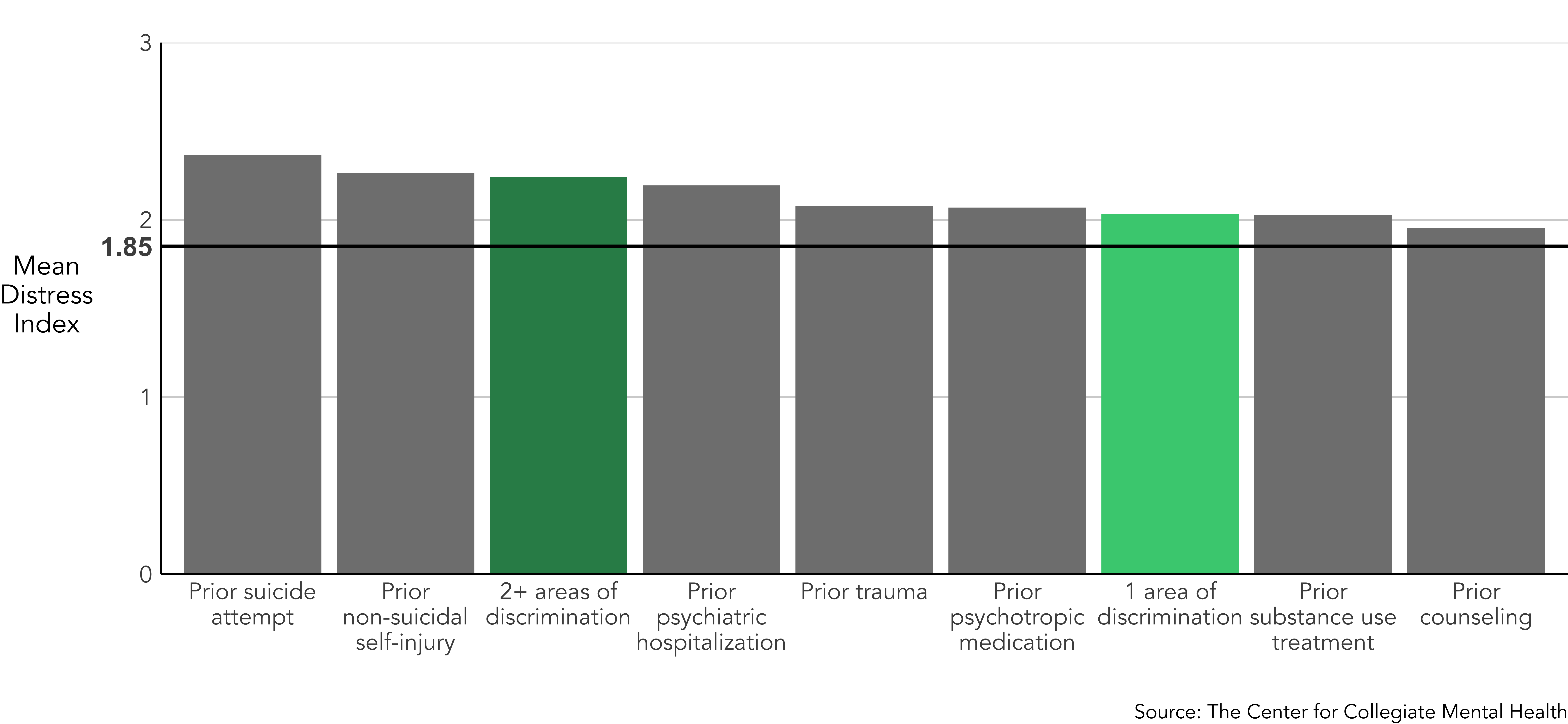
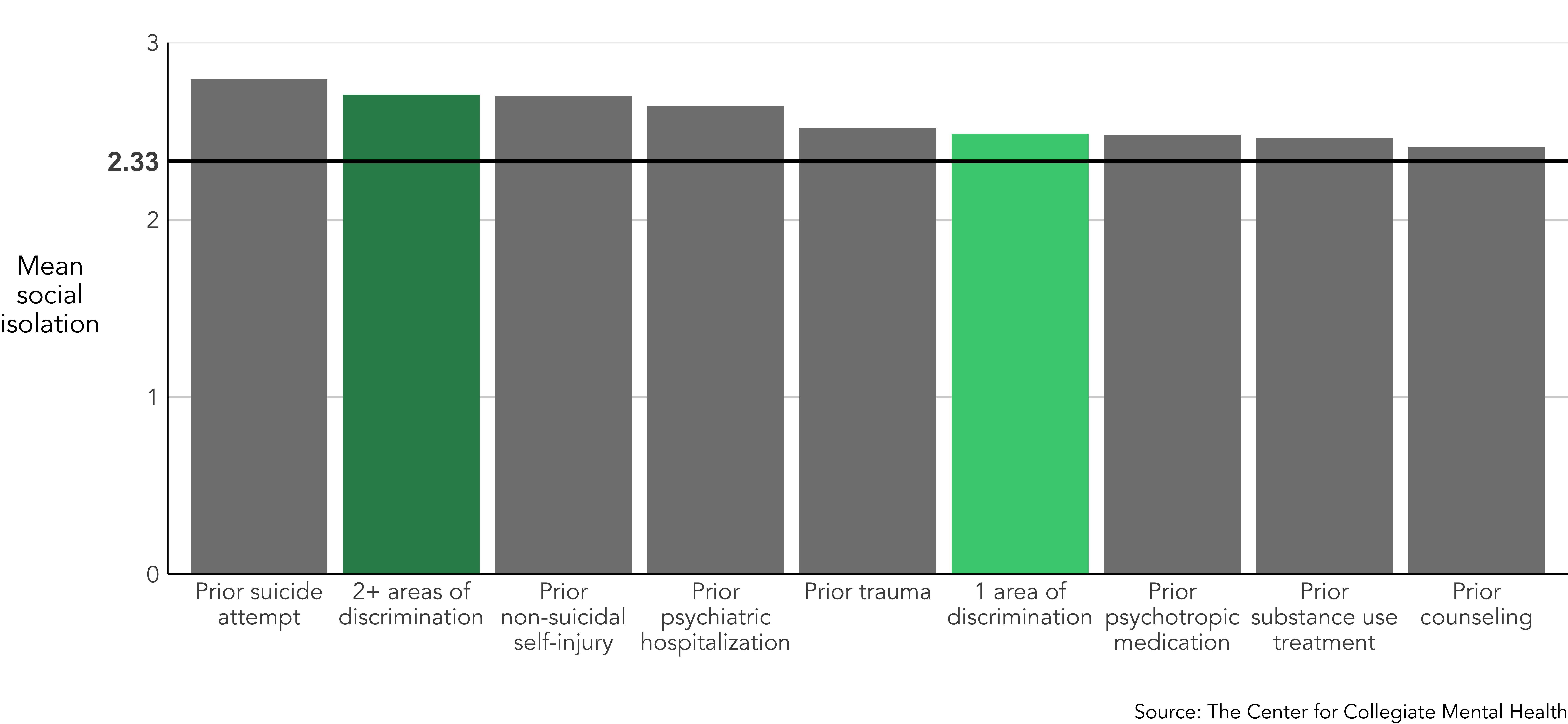
The symptom levels for students who endorsed any clinical history variables and/or discrimination were compared to the average rate of distress, social isolation, and suicidal ideation reported by clients when they begin college counseling services. This average level is indicated by the bold horizontal line within each figure. As expected, the rates of distress for every traditional clinical history variable were higher than the average, which clearly demonstrates the increased risk for elevated symptoms when students have a history of prior mental health treatment, trauma, and suicidal behavior. In the subsequent sections, levels of general distress, social isolation, and suicidal ideation were compared between clients who disclosed discrimination based on 1 or multiple (2+) identities and those who reported a history of the aforementioned key clinical variables.
General Distress
Similar to the historical clinical variables, students who experienced discrimination, notated by the green shaded bars, endorsed similar levels of general distress as students who disclosed prior mental health treatment, trauma, or threat-to-self behaviors. In particular, students who reported multiple (2+) areas of discrimination within the past six months displayed nearly the highest association to general distress, comparable to those with a history of a psychiatric hospitalization, non-suicidal self-injury, and a suicide attempt.
Social Isolation
Having a history of either 1 or multiple (2+) areas of discrimination was associated with elevated levels of social isolation. In fact, students who reported 2 or more areas of discrimination endorsed nearly the same level of social isolation as those who reported a past suicide attempt.
Suicidal Ideation
Students who experienced either 1 or multiple (2+) areas of discrimination disclosed suicidal ideation at similar levels to those who endorsed most of the other mental health history items. However, students who reported a prior suicide attempt had the highest rate of suicidal ideation.
COUNSELING CENTERS' ROLE IN SUPPORTING STUDENTS WITH EXPERIENCES OF DISCRIMINATION
Improvement in general distress, social isolation, and suicidal ideation (i.e., change between first and last administrations of the CCAPS) was compared between students who did and did not report discrimination. The changes were examined for all students, regardless of their level of symptoms at the beginning of treatment. The slope of the lines connecting first and last CCAPS administrations represents total improvement on that subscale, where steeper lines indicate more change. The numbers above or below each line indicate the average raw change in symptoms for each area of distress. Clients with experiences of discrimination began treatment (first administration) with higher levels of general distress, social isolation, and suicidal thoughts and showed similar improvement in all of these symptoms during counseling services compared to clients who did not indicate discrimination.
Despite notable improvement on each outcome (general distress, social isolation, and suicidal thoughts), students who disclosed discrimination still ended services (last administration) with considerably higher levels of distress than those who did not report discrimination. This outcome gap highlights the need for institutions to invest in and prioritize additional support services for students with discriminatory experiences.
SUMMARY
In the current 2023 Annual Report, CCMH investigated if experiences of discrimination or unfair treatment based on six identities are associated with mental health concerns and symptom improvement at college counseling centers. While we emphasized that discrimination is not a mental health diagnosis and rather a societal problem, this inquiry was considered critical given the findings could potentially assist clinicians in conceptualizing the environmental contexts that impact their clients and inform the support services delivered at college counseling centers, as well as the broader institutions.
The findings revealed that discrimination was strongly related to increased general distress, social isolation, and suicidal ideation, which was compounded when students disclosed multiple areas of discrimination. In fact, experiences of discrimination demonstrated associations with elevated symptoms equivalent to most historical clinical variables (i.e., history of suicide attempts, history of counseling) that clinicians have been trained to assess for decades. Moreover, counseling centers were shown to effectively treat clients with discrimination, as they, compared to students with no discrimination, demonstrated comparable improvement in symptoms of distress, social isolation, and suicidal ideation during services. While these findings highlight that counseling centers play an essential role in supporting students with recent discrimination, these clients consistently ended treatment with higher levels of distress, highlighting a persistent disparity in distress, social isolation, and suicidal ideation.
The findings underscore the critical function of gathering information pertaining to identity-based discrimination at the beginning of treatment. Although discrimination is not a mental health problem, it provides vital environmental and contextual information that is clearly associated with more severe mental health symptoms. Additionally, awareness and further assessment related to these experiences can potentially help clinicians better understand their clients in context, enhance the culturally affirmative support they provide during counseling services, advocate for their clients, and identify adjunctive services that might help students self-advocate and directly address their experiences of discrimination at the individual and systemic levels.
It is important to note several considerations related to the current findings. The strong association that was discovered between discrimination and mental health symptoms was correlational, and therefore causation between these variables can not be inferred. Additionally, the SDS item that inquires about discrimination neither specifies the source(s) of the discrimination nor the frequency of the experiences. Thus, it is unknown if the discrimination was experienced within the collegiate community or elsewhere, and how often it occurred. Finally, the current report did not specifically explore experiences of discrimination within various diverse demographic groups. In future investigations, it might be helpful to further assess the frequency and sources of discrimination, as well as the potential differential impacts of the various types of discrimination within specific identity groups. Nevertheless, this report provides a broad overview of the negative effects of discrimination, which emphasizes the importance of support services to address these affects at the individual and systemic levels of an institution.
The current findings highlight the critical role college counseling centers serve in supporting the Diversity, Equity, Inclusion, and Belonging (DEIB) goals that are a priority for many institutions. Students who have discrimination experiences are substantially more likely to report severe mental health symptoms, and college counseling services help these students feel less distressed, isolated, and suicidal. While counseling centers are effective in supporting DEIB initiatives in this manner, students who have experienced discrimination consistently end services with notably higher levels of distress than students without discrimination, creating an outcome gap or disparity. College counseling centers can effectively support these students; however, addressing the psychological symptoms is only a piece of the solution. Adjunctive DEIB informed support services (e.g., cultural centers, identity-based programs) are also essential to buffer the impact of discrimination, provide education/professional development to the campus community, and initiate advocacy to remedy campus and broader societal sources of discrimination. It is imperative for institutions to understand the close connection between DEIB and mental health. Institutions and leaders who prioritize and value mental health and wellness must concurrently support DEIB initiatives in order to reduce the disparities in mental health symptoms and treatment outcomes among students who face identity-based discrimination.
This post is a direct replication of the special section in our 2023 Annual Report, pages 5-9.
REFERENCES
- Oh, H., Stickley, A., Koyanagi, A., Yau, R., & DeVylder, J.E. (2019). Discrimination and suicidality among racial and ethnic minorities in the United States. Journal of Effective Disorders, 245, 517-523. doi. org/10.1177/00207640231175
- • Paradies, Y., Ben, J., Denson, N., Elias, A., Priest, N., Pieterse, A., Gupta, A., Kelaher, M., & Gee. G. (2015). Racism as a determinant of health: A systematic review and meta-analysis. PLOS ONE, 1-48. doi:10.1371/journal. pone.0138511

